| x | x | ||||
 |
|||||
| BACTERIOLOGY | IMMUNOLOGY | MYCOLOGY | PARASITOLOGY | VIROLOGY | |
|
|
INFECTIOUS DISEASE |
||||
|
|
|||||
|
|
|||||
|
Let us know what you think |
|||||
|
|||||
|
TEST YOUR KNOWLEDGE |
|||||
|
Overview of Skin
Infections Skin infections are best classified according to the nature of the lesion (e.g., macule, papule, vesicle, or pustule), the layer involved (Figure), and the microbial etiology. Certain of these infections, for example uncomplicated impetigo, can be treated in the primary setting without resort to special studies such as Gram’s stains and cultures. The clinician should be alert to the possibility of rare but serious lesions such as the membranous ulcers of cutaneous diphtheria or the malignant pustule of anthrax; of sexually transmitted diseases; and of the possibility that skin lesions signify underlying diseases.
|
|||||
|
Non-bullous Impetigo Impetigo is a common superficial infection of the epidermis usually encountered in children, typically on the face and extremities. In the past most cases of impetigo have been attributed to Streptococcus pyogenes (group A streptococcus). Group A streptococcal strains causing impetigo are, in general, of different M serotypes than those causing pharyngitis. In recent years S. aureus has emerged as the more common etiology at least in some localities. Group A streptococci and S. aureus are often encountered together, and asymptomatic carriage of either or both of these bacteria predisposes to impetigo. Some data suggest a prominent role for anaerobic bacteria. Group B streptococci can cause impetigo in newborn infants, and streptococci belonging to Lancefield groups C and G rarely cause this condition. Predisposing factors include warm, humid climates, poor personal hygiene, poverty, and minor skin trauma Impetigo typically involves exposed areas of the skin, especially the face but also the extremities. The initial lesions are small vesicles, which quickly become pustules and then rupture leaving a purulent discharge on the skin that dries to form honey-colored or golden-brown “stuck-on” crust. The lesions are painless but are often pruritic, prompting scratching which in turn spreads the infection to new areas. Mild lymphadenopathy is common, but high fever or other systemic symptoms should prompt a search for another diagnosis. The disease infects the most superficial layers of the epidermis. Impetigo is nearly always a self-limited disease that heals without scarring. However, it is a common cause of acute post-streptococcal glomerulonephritis, which is life threatening. |
|||||
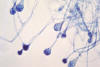 Figure 1
Figure 1Young sporangia of a Mucor spp. fungus. Mucor is a common indoor mold, and is among the fungi that cause the group of infections known as zygomycosis. The infection typically involves the rhino-facial-cranial area, lungs, GI tract, skin, or less commonly other organ systems.
|
Ecthyma Ecthyma resembles non-bullous impetigo in that it is usually caused by group A streptococci and/or staphylococci and begins as vesicles that become pustules which then rupture, leaving an exudates on the surface of the skin. In ecthyma, however, the process does not remain confined to the stratum corneum but rather extends through the epidermis. The result is typically a “punched-out” ulcer with raised violaceous margins. The ulcer is covered with a greenish yellow crust. The lesions are most commonly located on the lower extremities. Ecthyma occurs most frequently in young children and in the elderly. Unusual causes of ecthyma include cutaneous diphtheria, gonococcal infection, mucormycosis (figure 1-2), molluscum contagiosum (figure 3), and herpes simplex virus infection. This form of “uncomplicated ecthyma” must be distinguished from ecthyma
resulting from systemic infection (ecthyma gangrenosum). |
||||
 Figure 3 Histopathology of molluscum contagiosum, skin. CDC/Dr. Edwin P.
Ewing, Jr.
Figure 3 Histopathology of molluscum contagiosum, skin. CDC/Dr. Edwin P.
Ewing, Jr.
|
|||||
 Figure 4
Figure 4This patient presented with these gluteal lesions that proved to be impetigo, but was first thought to be syphilis. Impetigo is usually caused by Group A Streptococcus sp. or Staphylococcus aureus bacteria. Note how the maculopapular lesions resemble syphilis, which is caused by the Gram-negative Treponema pallidum spirochete. CDC |
Bullous Impetigo and the Staphylococcal Scalded Skin Syndrome Bullous impetigo is attributed to S. aureus strains belonging to phage group II capable of producing two extracellular exfoliative toxins (known as A and B) that separate the stratum corneum from the rest of the epidermis. The more common and milder form of the disease―representing about 10% of all cases of impetigo―differs from non-bullous impetigo in that the vesicles enlarge into flaccid bullae before rupturing (figure 4). The exposed skin surface is at first moist and red, resembling a small burn. A thin, light-brown, “varnish-like” crust then develops. The more severe form, which usually affects younger children, is known as the staphylococcal scalded skin syndrome. Widespread, flaccid bullae rupture causing exfoliation of the skin that resembles an extensive third-degree burn. This form of the disease can occur in epidemic form in nurseries, where it is known as pemphigus neonatorum or Ritter’s disease. Fever and other systemic symptoms are usually absent in the more localized forms of the disease but are invariably present in patients with the staphylococcal scalded skin syndrome. Staphylococcal scalded skin syndrome in adults is rare, and is usually associated with immunosuppression. Localized bullous impetigo is self-limited, but the staphylococcal scalded skin syndrome carries a significant mortality rate. |
||||
|
Folliculitis
|
|||||
 Figure 5
Figure 5Cutaneous abscess located on the hip, which had begun to spontaneously drain, releasing its purulent contents. The abscess was caused by methicillin-resistant Staphylococcus aureus bacteria, referred to by the acronym MRSA. CDC  Figure 6
Figure 6Cutaneous abscess located on the thigh, caused by methicillin-resistant Staphylococcus aureus bacteria. A clinician had lanced the lesion in order to allow the pus contained therein, to be released. CDC |
Furuncles, Carbuncles, and Skin Abscesses The familiar furuncle or “boil” is thought to arise from folliculitis. The term furunculosis refers to multiple boils or to frequent recurrences. Carbuncles are more extensive and difficult-to-treat lesions that often require surgical intervention. Skin abscesses, although similar to carbuncles histologically, are usually deeper infections that do not originate in hair follicles. S. aureus is the usual cause of both furuncles and carbuncles, and is also the sole or predominant pathogen in about 50% of skin abscesses (figure 5-6). Predisposing factors to recurrent furuncles (furunculosis) include obesity, corticosteroid therapy, disorders of neutrophil function, and possibly diabetes mellitus. Immunoglobulin levels are usually normal in patients with furunculosis (low IgM levels have been demonstrated in some patients but this is of uncertain significance and, in contrast to IgG deficiency, replacement therapy is impractical). Most patients with recurrent furuncles have no obvious predisposing factors other than being nasal carriers of S. aureus nasal carriers. Outbreaks of furunculosis have been described in families, athletic teams, and in village residents who took steam baths together. Skin abscesses can result from minor trauma, injecting drug use (the practice of subcutaneous and intramuscular injection is known as “skin popping”), or bacteremia. Congenital immunodeficiency syndromes such as the hyperimmunoglobulin E-recurrent infection syndrome (Job’s syndrome) are sometimes present in patients with recurrent skin abscesses. Rarely, skin abscesses are self-inflicted (factitious abscess), in which case Gram’s stain and culture may reveal “mouth flora” bacteria. Furuncles commonly present as tender, firm, round subcutaneous nodules. The
typical lesion is 1 to 2 cm in diameter, or about the size of a marble. The
overlying skin is often erythematous, but fever and other systemic signs of
illness are seldom present. Common sites for furuncles include the face, neck,
axillae, and buttocks, but any area of the body that contains hair follicles can
be affected.
|
||||
|
Hidradenitis Suppurativa Hidradenitis suppurativa is a chronic disease of the apocrine glands of the axillae (hidradenitis suppurativa axillaris), inguinal region (hidradenitis suppurativa inguinalis), and perianal skin. The lesions become secondarily infected, leading to abscesses, fistulas, and scarring. Surgery rather than antimicrobial therapy is the usual cure for severe cases. Although the basic cause is unknown, the mechanism of disease appears to be plugging of apocrine gland ducts by keratin. Pressure within the ducts causes them to dilate and rupture into the surrounding tissues. The initial inflammatory lesions are sterile, but bacterial superinfection quickly occurs. Pathogens that have been isolated include S. aureus, streptococci (including S. anginosus), aerobic gram-negative rods (such as E. coli, Proteus mirabilis, and Pseudomonas aeruginosa), and anaerobic bacteria. Early lesions consist of irregular reddish purple nodules, typically located in the axillae, groin, or perianal area. These lesions gradually enlarge and become fluctuant. Drainage results in sinus tracts. A foul odor to the drainage signifies anaerobic infection. In many patients the lesions remain, resolve or remain generally stable. Spontaneous resolution, however, is rare. In some patients, however, the disease progresses relentlessly resulting in extensive inflammation, undermining of the skin with sinus tracts, chronic drainage, and scarring. Complications tend to be more severe in the perineal and perianal forms of the disease and include fistulas and squamous cell carcinomas. |
|||||
 Figure 7
Figure 7Facial erysipelas manifested as severe malar and periorbital erythema and swelling. Note the purulent discharge from the eye. Erysipelas is a dermatologic condition, which involves the inoculation of the skin and subcutaneous tissue with streptococcal bacteria causing edema and bright red erythema of the affected areas. It is sometimes referred to as cellulitis. CDC/Dr. Thomas F. Sellers/Emory University
|
Erysipelas (Superficial Cellulitis) “Cellulitis” refers to spreading infection in the subcutaneous tissue. Erysipelas (figure 7 and 8) is a superficial form of cellulitis in which the involved skin assumes a fiery bright red color (hence the alternative name, “St. Anthony’s fire”). Group A streptococci (S. pyogenes) cause most cases of erysipelas. Group B
streptococci cause some cases of erysipelas in newborn infants, and streptococci
belonging to groups C and G have caused streptococci in adults. In one study,
more than 96% of cases of erysipelas were attributed to streptococci on the
basis of extensive studies that included cultures of punch biopsy specimens.
Rarely, S. aureus causes erysipelas. |
||||
|
Cellulitis (Other Than Erysipelas) Cellulitis other than erysipelas is a deeper infection of the subcutaneous tissue usually caused by streptococci, staphylococci, or both. However, the etiologic spectrum is diverse. Cellulitis usually results from introduction of a pathogen into the skin by way of a wound or pre-existing skin lesion. Examples of the former include cuts and punctures; examples of the latter include ulcers (such as stasis ulcers or decubiti), eczema, or furuncles. Predisposing factors include tinea pedis, peripheral vascular disease, peripheral edema including lymphedema, prior history of cellulitis, and diabetes mellitus. S. pyogenes (group A streptococci) and S. aureus are the usual etiologies, but careful studies have established that cellulitis is often a mixed infection involving both of these microorganisms. A large and growing number of microorganisms have been associated with cellulitis, including the following with therapeutic implications:
|
|||||
|
Membranous Ulcers Including Cutaneous Diphtheria Cutaneous ulcers such as those associated with venous or arterial insufficiency in the lower extremities are relatively common. Occasionally, such an ulcer manifests at its base a layer of necrotic debris resembling a membrane. Analysis of the associated purulent drainage, which is often abundant, usually discloses a mixture of various aerobic and anaerobic bacteria. Rarely, such ulcers are caused by cutaneous diphtheria, which is now the most common form of diphtheria reported in the U.S. and which serves as a reservoir for transmission of the disease. A majority of confirmed cases in the U.S. in recent years have been imported from other countries, but vulnerable populations include homeless persons, Native Americans, and certain populations in the Southeastern states and the Pacific Northwest. Primary cutaneous diphtheria presents as an indolent, non-healing, “punched-out” skin ulcer with a dirty-gray or gray-brown membrane at its base. Wound diphtheria involves secondary infection of a preexisting wound, all or part of which becomes covered by a membrane. Suspicion of cutaneous diphtheria should prompt attempts to make a definitive diagnosis by culture and to demonstrate the presence of the toxin by special methods. All cases of suspected or confirmed diphtheria should be reported promptly to the local health department.
|
|||||
|
Pyomyositis Pyomyositis, an acute pus-forming infection of skeletal muscle, was in the past usually called “tropical pyomyositis” to denote its geographic association. Recent reports indicate that pyomyositis is becoming more common in the U.S. and other developed countries. These reports also emphasize an association with HIV disease and with injecting drug use, but some patients have no obvious predisposing condition. S. aureus causes about 95% of cases in tropical areas and about two-thirds of cases in the United States. Streptococci (most often group A streptococci but also groups B, C, and G, S. pneumoniae, and S. anginosus) are as a group the second most common cause in the United States. A history of recent blunt trauma or unusual exertion is obtained in up to one-half of patients with pyomyositis, suggesting that local muscle injury created a “place of least resistance” (locus minoris resistentiae) that was subsequently infected during what would otherwise have been a transient, self-limited bloodstream infection. Whereas most patients with tropical pyomyositis have no underlying disease, about 60% of patients with pyomyositis in temperate climates have a defect in host defenses. Pyomyositis usually affects the large muscles of the lower extremities or trunk. The illness typically unfolds over several weeks. Most patients present with pain and tenderness localized to the body of a muscle, but an occasional patient will present with an acute illness with marked systemic toxicity. Unusual presentations include toxic shock syndrome and infection of the abdominal wall resembling the presentation of acute abdomen. Untreated, pyomyositis often progresses to severe sepsis with shock and death.
|
|||||
 Figure 9
Figure 9The foot of this patient is swollen due to gonococcal arthritis. Gonorrhea is the most frequently reported communicable disease in the U.S. Disseminated gonococcal infection is most often the cause of acute septic arthritis in sexually active adults, and the reason for most hospitalizations due to infective arthritis. CDC  Figure 10
Figure 10This patient presented with cutaneous foot lesions that were diagnosed as a disseminated gonococcal infection. CDC |
Acute Septic Arthritis (Acute Infectious Arthritis) Here, the term septic arthritis will be used for acute infectious arthritis of bacterial etiology. This condition is uncommon in the general population (annual incidence 2 to 5 per 100,000 persons), but is more common in patients with rheumatoid arthritis (28 to 38 per 100,000) and in persons with a joint prosthesis (40 to 68 per 100,000). The disease usually affects a single joint, most commonly the knee. S. aureus is the most common pathogen, but special note should be taken of N. gonorrhoeae in sexually active young adults and of a wide range of bacteria under special circumstances. Septic arthritis usually results from hematogenous seeding of the synovium, a highly vascular tissue that lacks a basement membrane. Especially vulnerable patients include young infants because of the rich vascularity surrounding their epiphyseal growth plates and patients with chronic arthritis, joint implants, recent trauma, or chronic debilitating diseases including the frail elderly. Septic arthritis can also be secondary to penetrating trauma. Septic arthritis of the hands and wrists is commonly caused by trauma including animal and human bites. In newborn infants the usual etiologies are group B streptococci, aerobic gram- negative rods, and S. aureus. H. influenzae type b was formerly the usual cause of septic arthritis in toddlers, but wide use of the conjugate vaccine has virtually eliminated this disease. Kingella kingae, a fastidious gram-negative rod, is emerging as an important joint pathogen in children. After age 2, S. aureus becomes the most common cause of septic arthritis in persons other than sexually active young adults, in whom gonococcal arthritis (figure 9) is common. Streptococci (not only group A but also groups B, C, and G) are relatively common causes. Pasteurella multocida causes particularly aggressive disease after a cat bite. Aerobic gram-negative rods cause up to one-fifth of cases, usually in the setting of chronic underlying disease or injection drug use. Streptococcus pneumoniae occasionally causes septic arthritis, especially in children with sickle cell disease. A wide variety of bacteria cause occasional cases. Septic arthritis due to Pseudomonas aeruginosa and occurring in unusual places (e.g., sternoclavicular joints, sacroiliac joints, or pubic symphysis) is well documented among injecting drug users. Acute septic arthritis usually presents with pain, swelling, and limitation of motion of the affected joint. Most patients are febrile. A single large joint is involved in about 90% of children and about 80% to 90% of adults. The knee is the most commonly involved joint, followed by the hip and the shoulder. Patients with rheumatoid arthritis are more likely to have multiple joint involvement. Patients with gonococcal arthritis also have involvement of multiple large and small joints, but on closer inspection there is often little or no joint effusion despite prominent inflammation of the adjacent tendons (tenosynovitis). Associated vesiculopustules strongly suggest the gonococcal arthritis-dermatitis syndrome. |
||||
|
Septic Bursitis Septic bursitis most commonly involves the olecranon or prepatellar bursae. S. aureus causes most cases of acute septic bursitis; chronic cases can be due to a wide range of microorganisms. Minor trauma is likely to be a precipitating factor, especially when bursae of the lower extremities are involved. Chronic infectious bursitis, which typically follows minor trauma, is associated with a wide variety of bacteria and fungi of low virulence. Examples include fungi that are soil contaminants and non-tuberculous mycobacteria. Septic bursitis presents with some combination of pain, tenderness, erythema, warmth, and swelling over the affected bursa in a person vulnerable to recurrent trauma such as a painter or brick mason. The presentation may be acute when due to S. aureus or subacute or chronic when due to an organism of lesser virulence. Absence of pain on movement of the joint helps distinguish septic bursitis from arthritis. Although septic bursitis is an uncommon lesion, the diagnosis is easily made on clinical grounds when suspected and confirmed by aspiration or open exploration of the bursa. |
|||||
|
Viral Arthritis Arthritis, usually symmetric and self-limited, is a prominent feature of several viral infections. Most cases result from viral invasion of the synovium and/or deposition of circulating immune complexes. Presentations vary according to the etiology:
|
|||||
 Figure 11
Figure 11This patient’s arm shows the effects of the fungal disease sporotrichosis, caused by the fungus Sporothrix schenckii. The first symptom is usually a small painless bump that’s red, pink, or purple. This is followed by one or more additional bumps/nodules which open and may resemble boils. Eventually lesions look like open sores, or ulcerations, and heal slowly. CDC/Dr. Lucille K. Georg |
Chronic Monoarticular Arthritis due to Infection Chronic arthritis involving a single joint, when due to infection, is usually caused by mycobacteria (including M. tuberculosis), fungi, nocardia, brucellosis, or Whipple’s disease. Most cases of chronic monoarticular arthritis arise by hematogenous infection. Sporothrix schenckii (sporotrichosis) (figure 11) is perhaps the most common fungal etiology in non-immunocompromised patients and most often involves the knee. Brucella species are notorious causes of chronic arthritis in parts of the world where brucellosis remains prevalent. Whipple’s disease, recently attributed to a bacterium named Tropherma whippelii, can also cause chronic monoarticular arthritis. |
||||
|
Acute Hematogenous Osteomyelitis Hematogenous osteomyelitis results when microorganisms enter the bloodstream from a distant source (such as a minor skin lesion), enter bone through a nutrient artery, and establish infection. The disease occurs most often in infants and children, but can occur at any age group. Hematogenous osteomyelitis in adults most often involves the spine (vertebral osteomyelitis) and is discussed separately. Acute hematogenous osteomyelitis is nearly always caused by a single organism. S. aureus is common in all age groups and is the most common cause in adults. Group B streptococci and E. coli commonly cause the disease in infants, and group A streptococci often cause the disease in older children. H. influenzae was a common cause of osteomyelitis in young children before the wide use of the vaccine. Salmonella species not infrequently cause hematogenous osteomyelitis in patients with sickle cell disease or other hemoglobinopathies. The occurrence of hematogenous osteomyelitis is best explained by the fragile nature of the arterial supply to the metaphyseal regions of bones, and especially those of growing children. Minor trauma such as the “lumps and bumps” of childhood disrupts the delicate capillary loops of these regions, causing small areas of necrosis that provide safe harbors for any bacteria that chance to come their way through the bloodstream. In infants less than 1 year of age, the growth plates of bone have a rich blood supply and therefore hematogenous osteomyelitis often affects the epiphyses of long bones. Thereafter the growth plates lose their blood supply, causing osteomyelitis to be confined to the metaphysis and diaphysis. Symptoms vary according to age but can be subtle in all age groups. In neonates, findings often consist of localized swelling and decreased motion in an extremity, often (about 60% of cases) accompanied by an effusion in the adjacent joint. About one-half of children with osteomyelitis present with an acute or subacute illness over several weeks with fever and other constitutional symptoms accompanied by signs of inflammation over the affected bone. In many children and in most adults, the illness evolves over a month or longer with vague constitutional symptoms and non-specific bone pain. |
|||||
|
Vertebral osteomyelitis and diskitis Vertebral osteomyelitis typically involves two adjacent vertebrae and the intervertebral disk; when the disk alone is involved the process is called diskitis. Vertebral osteomyelitis often presents as a subacute or chronic illness with constitutional symptoms and localized back pain. Occasionally, it presents as acute fever with back pain. Fever is absent in about one-half of patients. Complications include paraspinous abscess, epidural abscess, and spinal cord compression. Neurologic symptoms such as weakness in the lower extremities or impaired bladder or bowel function indicate spinal cord compression. The disease occurs mainly in adults. In children, the initial complaint is usually refusal to walk, a limp, or back pain. Most cases are of hematogenous origin, but occasional cases result from
inoculation of bacteria during spinal surgery, lumbar puncture, myelography, or
other medical procedures. S. aureus is the most common pathogen. Aerobic
gram-negative rods are relatively common causes especially in patients with
chronic urinary tract infections. Tuberculosis of the spine (Pott’s disease)
should always be considered. Occasional cases are caused by fungi or unusual
pathogens. |
|||||
|
Osteomyelitis Following Nail Puncture Wounds Nail puncture wounds can result in various combinations of cellulitis, abscess, osteochondritis, septic arthritis, and osteomyelitis. Osteomyelitis complicates about 1% to 2% of nail puncture wounds in children. Most of these infections occur during the warm summer months. Osteomyelitis due to Pseudomonas aeruginosa is strongly associated with wearing tennis shoes at the time of the injury (up to 93% of cases). Staphylococcus aureus is the other major pathogen, and in one series both Ps. aeruginosa and S. aureus were isolated in about one half of the cases. |
|||||
|
Infections of the Hand Acute paronychia, usually caused by S. aureus, is an infection involving the lateral fold of soft tissue surrounding the fingernail. Trauma to the nail including nail biting, foreign bodies, manicures, or hangnail is the usual predisposing cause. Injury to the seal between the nail plate and the nail fold allows bacteria to enter, causing cellulitis and/or the abscess. Herpes whitlow, caused by the herpes simplex virus (HSV-1 or HSV-2), usually involves the fingertip including structures related to the nail bed. This lesion is an occupational hazard for health care workers, being encountered not infrequently among nurses, surgeons, and dentists. Patients with herpetic gingivostomatitis and genital herpes are also at risk. Chronic paronychia is usually associated with Candida albicans (about 95% of cases) but a wide range of bacterial, fungal, and mycobacterial pathogens have been recovered. There is typically a history of frequent immersion of the hands in water. Persons at risk include housewives, dishwashers, swimmers, bartenders, and persons with diabetes mellitus or who are immunosuppressed. The condition most commonly affects women between the ages of 30 and 60 years. Recurrent episodes of pain, inflammation, and swelling eventually lead to chronic induration around the nail, often involving the eponychium (the thin membrane on the proximal aspect of the nail that serves as a seal between the nail wall and the nail plate). |
|||||
|
|
|||||


