|
x |
x |
|
 |
 |
|
INFECTIOUS
DISEASE |
BACTERIOLOGY |
IMMUNOLOGY |
MYCOLOGY |
PARASITOLOGY |
VIROLOGY |
|
|
Please Note: A new expanded and
updated version of this page is now available
Please go
here
MYCOLOGY - CHAPTER FIVE
FILAMENTOUS
FUNGI
Dr Art DiSalvo
Emeritus Director, Nevada State Laboratory
Emeritus Director of Laboratories, South Carolina Department of Health
and Environmental Control
|
|
TURKISH |
|
SHQIP-ALBANIAN |
Let us know what you think
FEEDBACK |
|
SEARCH |

 |
|
|
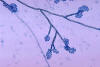
 Figure 1.
Figure 1.
This slide culture of the fungus Fonsecaea pedrosoi, revealed the
presence of a phialide with accompanying phialospores. Fonsecaea
pedrosoi is one of the etiologic pathogens responsible for the
infection known as chromoblastomycosis, especially in the more humid
regions of the world. Normally it is found amongst rotting woods and soil
debris.
CDC/Dr. Lucille K. Georg |
CHROMOBLASTOMYCOSIS
This is a chronic,
localized infection infection of subcutaneous tissues caused by several species
of dematiaceous fungi. The 3 most common agents are:
- Fonsecaea pedrosoi (figure 1)
- Cladosporium carrionii (figure
2 and 4)
- Phialophora verrucosa (figure
3)
These fungi, recognized by a variety of
names, are saprobes located in soil and decaying vegetation. The route of entry
is usually by trauma. The lesions are sub-cutaneous and the surface can be flat
or verrucous (figure 4A). The lesions take several years to develop. These organisms are
called dematiaceous fungi, because they have a black color in the mycelium cell
wall (in culture and in tissue). In tissue these fungi form sclerotic bodies
which are the reproductive forms dividing by fission (figure 4B). These organisms induce a granulomatous reaction. The etiologic agents of chromoblastomycosis are septate,
mold-like, branching, darkly pigmented which produce asexual fruits called
conidia. We identify these fungi in culture by the shape and formation of the
conidia. The fungi have a world-wide distribution especially in warmer climates
like the tropics or the southern U.S. The melanin in the pigment may be a
virulence factor. These organisms are distributed world-wide. There is no really
successful therapy. Excision and local heat have been used with some success.
Flucytosine (5-FC) and itraconazole have also been used to treat
(or control) this disease. Posaconazole is showing some promise as a therapeutic
agent. There are no serological tests to aid in the diagnosis.
|
 Figure 2
Figure 2
Cladosporium (Cladophialophora) carrionii, magnified 475X. The
C. carrionii fungus is a common cause of chromoblastomycosis
infections, and is particularly prevalent in arid and semi-arid areas,
most often in tropical and subtropical zones.
CDC/Dr. Lucille K.
Georg |
 Figure 3
Figure 3
Conidia-laden conidiophores of a
Phialophora verrucosa fungal organism
from a slide culture. Note the flask-shaped phialides, each lipped by a
collarette. Each phialide terminates in a bundle of round, to ovoid conidia. Phialophora spp. are known to be a cause of both chromoblastomycosis, and
phaeohyphomycosis. CDC/Dr. Libero Ajello
 Figure 4
Figure 4
Plate culture of
Cladosporium carrionii, at four weeks growth. C.
carrionii infection is a common cause of chromoblastomycosis, and is
particularly prevalent in arid and semi-arid areas, most often in tropical and
subtropical zones. CDC/Dr. Lucille K. Georg
 Figure 4A
Figure 4A
Chromoblastomycosis lesions are sub-cutaneous and the surface can be flat
or verrucous
Dr Arthur DiSalvo
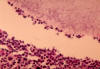
 Figure 4B
Figure 4B
Dematiaceous fungi:
In tissue
these fungi form sclerotic bodies which are the reproductive forms dividing by
fission
Dr Arthur DiSalvo
|
 Figure 5.
Figure 5.
Black grain mycetoma: subcutaneous nodule due to Madurella Mycetomatis, magnified x 100
© Bristol Biomedical Image Archive. Used with permission
 Figure
6. Figure
6.
Mycetoma with presence of geotrichum
© Bristol Biomedical Image Archive. Used with permission |
MYCETOMA
(Maduromycosis)
Mycetomas (fungous tumors) are also
chronic, subcutaneous infections (figure 5). These are called eumycotic mycetoma (tumors
caused by the TRUE fungi as opposed to those caused by actinomycetes) (figure 6). These
tumors frequently invade contiguous tissue, particularly the bone. A diagnosis
of the etiologic agent is essential for patient management because the prognosis
and therapy differs. Mycetoma characteristics:
1. tumefaction - swelling
2. granules - a variety of colors (white,
brown, yellow, black)
3. draining sinus tracts
The three most common etiologic agents
are:
1. Madurella mycetomatis (figure 7
and 8)
2. *Exophiala jeanselmei (figure 9)
3. *Pseudallescheria boydii (figure
10 and 11)
*The most common in the US. These organisms
are associated with the soil, thus you see many infections in the feet and legs.
Clinical specimens for diagnosis:
1. pus - with granules
2. tissue - for histological examination
The color, size and texture of the
granules are an aid in the diagnosis of mycetomas. The agents of mycetoma are all
filamentous fungi which require 7-10 days for visible growth on the culture
media and then another several days for specific identification. These fungi are
identified by the colonial morphology, conidia formation and biochemical
reactions. The species of fungi cannot be distinguished in histopathological
tissue sections. Treatment is very difficult, but terbinafine and itraconazole
have been used with some success. Posaconazole seems to be efficacious.
|
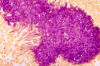 Figure 7.
Figure 7.
Histopathologic appearance of “black grain mycetoma” due to Madurella
mycetomatis using a Gridley stain. “Black grain mycetoma”, though
usually a localized infection, can involve not only the superficial layers
of skin, but underlying fascia and bones as well, with the fungal pathogen
entering the body through a traumatic wound.
CDC/Dr. Libero Ajello |
 Figure 8.
Figure 8.
Specimen of fibroadipose tissue containing “black grain” mycetoma due to
the fungus Madurella grisea. Some Madurella spp. are a cause
of mycetoma, a fungal infection characterized by sclerotia, or large black
masses of hyphae. The fungus enters the human body via trauma, which
usually affects the foot. This disease process may take several years.
CDC
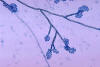 Figure 9.
Figure 9.
Conidiophores of the fungus Exophiala jeanselmei. Exophiala
jeanselmei, is a well documented human pathogen. Clinical
manifestations include mycetoma, localized cutaneous infections,
subcutaneous cysts, endocarditis, cerebral involvement, and systemically
disseminated infections. CDC/Dr. Libero Ajello.
 Figure 10.
Figure 10.
Conidiophores with conidia of the fungus Pseudallescheria boydii
from a slide culture. Pseudallescheria boydii is pathogenic in
humans, especially those who are immunocompromised, causing infections in
almost all body regions, and which are classified under the broad heading
of “Pseudallescheriasis”. CDC/Dr. Libero Ajello
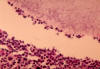 Figure 11.
Figure 11.
Eumycotic mycetoma due to the fungus Pseudallescheria boydii.
Pseudallescheria boydii is the most common etiologic agent associated
with eumycetoma in the United States. The disease is a chronic cutaneous
and subcutaneous infection with the foot being the most common site for
lesions. CDC/Dr. Hardin
|
 Figure 12.
Figure 12.
Histopathologic changes seen in zygomycosis due to Rhizopus arrhizus
using FA stain technique. Rhizopus arrhizus, the most common
Rhizopus spp., is known to be the cause of zygomycosis, an angiotropic
disease, which means that it tends to invade the blood vessels, thereby,
facilitating its systemic dissemination.
CDC/Dr. William
Kaplan
 Figure 13.
Figure 13.
Histopathologic changes seen in a heart valve due to zygomycosis caused by
Mucor pusillus. Using methenamine silver stain, one can detect the
presence of fungal elements associated with zygomycosis, including
sparsely septate hyphae, amongst a mostly acute inflammatory process with
some island of chronic granulomatous inflammation.
CDC/Dr. Libero
Ajello
 Figure 14
Figure 14
Mucor sp. enter the brain via the blood vessels
Dr Arthur DiSalvo |
MUCORMYCOSIS
Also known as
zygomycosis and phycomycosis. Mucormycosis is an acute inflammation of soft
tissue, usually with fungal invasion of the blood vessels. This rapidly fatal
disease is caused by several different species in this class. The zygomycetes,
like the Candida species, are ubiquitous and rarely cause disease in an
immunocompetent host. Some characteristic underlying conditions which cause
susceptibility are: diabetes, severe burns, immunosuppression or intravenous
drug use.
The three most common genera causing this clinical entity are:
- Rhizopus species (figure 12)
- Mucor species (figure 13)
- Absidia species
Characteristics
These fungi are found world-wide,
commonly in soil, food, organic debris etc. They are seen on decaying vegetables in the
refrigerator and on moldy bread. Rhinocerebral infections are common. This
disease is frequently seen in the uncontrolled diabetic patients.
Typical case
An
uncontrolled diabetic patient comes to ER (may be comatose depending on the
state of diabetes) and a cotton-like growth is observed on the roof of the mouth
or in the nose. These are the hyphae of the organism. If untreated, the patient
will die within a few hours or days. What do you do to help this patient first?
Controlling the diabetic state is most important before administering
amphotericin.
These fungi have a tendency to invade
blood vessels (particularly arteries) and enter the brain via the blood vessels
and by direct extension through the cribiform plate (figure 14). This is why they cause
death so quickly.
Culture
A rapid growing, loose, white
mold is visible within 24 to 48 hours. With age, and the formation of sporangia,
the colony becomes dark gray. The sporangia contain the dark spores (figure 16). The
mycelium is wide (10-15 microns), ribbon-like and non-septate (coenocytic).
This same appearance is clear in tissue sections. The species are identified by
the morphology in culture.
Treatment
Treatment consists of debridement and amphotericin
Identification
There is an immunodiffusion test
available, but the physician cannot wait for these results before instituting
rapid, vigorous intervention. The diagnosis and treatment must be immediate and
based primarily on clinical observations.
|
 Figure 15
Figure 15
This patient presented with a case of a periorbital fungal infection known
as mucormycosis, or phycomycosis. Mucormycosis is a dangerous fungal
infection usually occurring in the immunocompromised patient, affecting
the regions of the eye, nose, and through its growth and destruction of
the periorbital tissues, it will eventually invade the brain cavity.
CDC/Dr.
Thomas F. Sellers/Emory University |
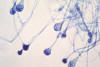 Figure 16
Figure 16
Young sporangia of a Mucor spp. fungus.
Mucor is a common indoor
mold, and is among the fungi that cause the group of infections known as
zygomycosis. The infection typically involves the rhino-facial-cranial area,
lungs, GI tract, skin, or less commonly other organ systems.
CDC/Dr. Lucille K. Georg
|
 Figure 16
Figure 16
Conidia: phialoconidia of Aspergillus fumigatus CDC
 Figure 17
Figure 17
This photomicrograph shows the conidial head of an Aspergillus niger
fungus. Conidial heads of Aspergillus niger are large, globose, and
dark brown, and contain the fungal spores, facilitating propagation of the
organism. This is one of the most common species associated with invasive
“pulmonary aspergillosis”.
CDC/Dr. Lucille K. Georg
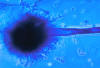 Figure 18
Figure 18
This photomicrograph depicts the appearance of a conidiophore of the
fungus Aspergillus flavus. Aspergillus spp. are filamentous,
cosmopolitan and ubiquitous fungi found in nature, are commonly isolated
from soil, plant debris, and indoor air environments, and are the most
commonly isolated filamentous fungi in invasive infections.
CDC/Dr. Libero
Ajello
|
ASPERGILLOSIS
Aspergilli produce a wide
variety of diseases. Like the zygomycetes, they are ubiquitous in nature and
play a significant role in the degradation of plant material as in composting.
Similar to Candida and the Zygomycetes, they rarely infect a normal host. The
organism is distributed world-wide and is commonly found in soil, food, paint,
air vents. They can even grow in disinfectant. There are more than one hundred
species of aspergilli The most common etiologic agents of aspergillosis in the
United States:
- Aspergillus fumigatus (figure
16)
- Aspergillus niger (figure 17)
- Aspergillus flavus (figure 18)
There are three clinical types of
pulmonary aspergillosis:
- Allergic hypersensitivity to the
organism. Symptoms may vary from mild respiratory distress to alveolar fibrosis.
- Aggressive tissue invasion.
Aspergillosis is primarily a
pulmonary disease, but the aspergilli may disseminate to any organ. They may
cause endocarditis, osteomyelitis, otomycosis and cutaneous lesions.
- Fungus ball which is
characteristically seen in the old cavities of TB patients. This is easily
recognized by x-ray (figure 19), because the lesion (actually a colony of mold growing in
the cavity) is shaped like a half-moon (semi-lunar growth). The patients may
cough up the fungus elements because the organism frequently invades the
bronchus. Chains of conidia can sometimes be seen in the sputum.
Culture
Aspergilli require 1-3 weeks for growth. the colony begins as a dense white
mycelium which later assumes a variety of colors, according to species, based on
the color of the conidia. The hyphae are branching and septate. Species
differentiation is based on the formation of spores as well as their color,
shape and texture.
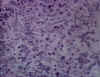
Histopathology
The septate hyphae are wide and form
dichotomous branching, i.e., a single hypha branches into two even hyphae, and
then the mycelium continues branching in this fashion (figure 20).
Serology
There is an
excellent serological test for aspergillosis which is an Immunodiffusion test.
There may be 1 to 5 precipitin bands. Three or more bands usually indicate
increasingly severity of the disease. i.e., tissue invasion.
Treatment
Voriconazole and Amphotericin B.
|
 Figure 19
Figure 19
This chest radiograph shows probable aspergillosis with an aspergilloma,
or fungus ball in the upper lobe of the right lung. Lung diseases that
damage a lung can cause cavities that can leave a person more susceptible
to developing an aspergilloma, or fungus ball. The fungus can then begin
secreting toxic and allergic products, which may make the person feel ill.
CDC/M. Renz
 Figure 20
Figure 20
Branching of aspergillus hyphae
Dr Arthur DiSalvo
|
 Aspergillosis. Human mouth. Gomori's silver methenamine stain
©
Bristol Biomedical Image Archive. Used with permission
Aspergillosis. Human mouth. Gomori's silver methenamine stain
©
Bristol Biomedical Image Archive. Used with permission
 Lung: Aspergillus hyphae in fungal pneumonia
©
Bristol Biomedical Image Archive. Used with permission
Lung: Aspergillus hyphae in fungal pneumonia
©
Bristol Biomedical Image Archive. Used with permission
 Fungal granulomas in lung caused by Aspergillus fumigatus
©
Bristol Biomedical Image Archive. Used with permission
Fungal granulomas in lung caused by Aspergillus fumigatus
©
Bristol Biomedical Image Archive. Used with permission
 Aspergillus pneumonia in lung of deer
© Bristol
Biomedical Image Archive. Used with permission
Aspergillus pneumonia in lung of deer
© Bristol
Biomedical Image Archive. Used with permission
 Nasal aspergillosis © Bristol Biomedical Image
Archive. Used with permission
Nasal aspergillosis © Bristol Biomedical Image
Archive. Used with permission
|
| |
|
| |
 Return to the Mycology Section of Microbiology and Immunology On-line
Return to the Mycology Section of Microbiology and Immunology On-line
This page last changed on
Sunday, December 30, 2018
Page maintained by
Richard Hunt
|
 Figure 1.
Figure 1. Figure 2
Figure 2 Figure 5.
Figure 5.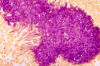 Figure 7.
Figure 7. Figure 12.
Figure 12. Figure 15
Figure 15 Figure 16
Figure 16 Figure 19
Figure 19